BIO 102 MENU
syllabus 
1 - origin 
2 - biomol. 
3 - biomol2 
4 - viruses
5 - prokaryon 
6 - endosym 
7 - eukaryon 
8 - energy 
9 - mitosis 
10 - meiosis 
11 - reprod 
12 - genetics 
13 - humgene 
14 - humge2 
15 - evolution 
16 - evolutio2 
17 - diversity 
18 - diversi2 
19 - tissues 
20 -digestive 
21 - respirat 
22 - circul 
23 - excret 
24 - endocr 
25 - receptors 
26 - nervsys 
Quizzes
Bio 103 Lab 
(full title of lecture appears in status bar on the top or at the bottom of your window)
Biology 102 - General Biology
Human Genetics II
Complex Traits: Multifactorial
The type of inheritance we have been discussing is called simple Mendelian inheritance and the traits we have discussed are controlled by genes at a single locus. Many traits are multifactorial. This means they are controlled by genes at several loci which may be additive (polygenic) and other genes and the environment also play a role in the expression of the trait.
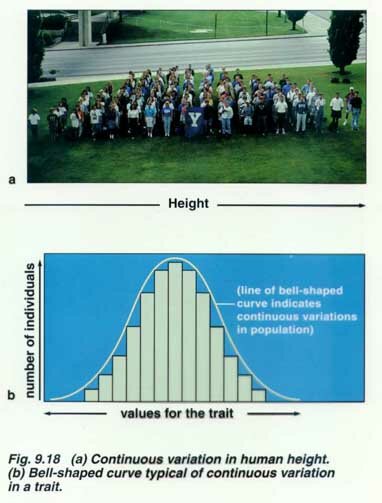
Examples of multifactorial traits include height, skin color, cleft lip and neural tube defects. If we use height as an example, we can say it is controlled by additive genes at four different loci. If you get all eight alleles for "tallness" you will be a one extreme of height, if you get eight alleles for "shortness" you will be at the other end of the height spectrum. If we lined everyone up according to height, they would fall into a bell-shaped curve with most being of medium height. Other factors influence height. There are genes on the X and Y chromosomes for height and people with extra X's or Y's are taller. Nutrition also plays a role. For example, you can see that second generation immigrants are taller than their parents if their parents came from a situation where they were not as well fed. Also, males are taller than females due to hormonal effects. Other genes can overcome the genes for height. For example, an achondroplasia gene will cause a person to be short independent of their genes for height.
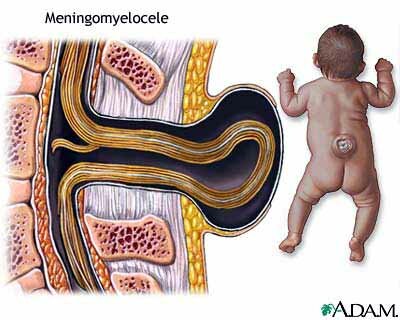
Neural Tube Defects
Neural tube defects (NTD) such as anencephaly and spina bifida and also cleft lips are examples of multifactorial traits which show a threshold effect. This means you need a certain number of genes for NTD before the trait manifests itself in the phenotype. Folate, a vitamin, is an environmental agent which can affect the expression of the genes for NTDs. All of us carry some of these genes and depending on how many are carried by our partner and how many each gives to the sperm or egg, we may have affected children. If you are affected or a first degree relative is affected or if you have an affected child, you are at a higher risk than the general population risk for having an affected child because you probably have more of these genes.
Normal Human Chromosomes
Humans normally have 46 chromosomes, 23 pairs. We get 23 from our mothers and 23 from our fathers. Mothers give 22 autosomes (1-22) and an X chromosome. Fathers give us 22 autosomes and either and X or a Y chromosome. The father determines the sex of his offspring. If the sperm contains an X chromosome, the baby will be a girl. If the sperm contains a Y chromosome, the baby will be a boy. The Y chromosome has a gene called the SRY which determines maleness. Each chromosome (except the Y) has a partner with which it pairs during meiosis which is the formation of the gametes (eggs and sperm). During mitosis which forms the baby, the chromosomes do not need a partner (see lecture on Mitosis and Meiosis).


NORMAL FEMALE KARYOTYPE (46,XX) AND NORMAL MALE KARYOTYPE (46,XY)
Chromosome Abnormalities (e.g. Down syndrome)
Another type of human genetic disorder involves chromosome abnormalities. If the chromosomes do not separate as they should in meiosis, the egg or sperm can receive more or fewer chromosomes than they should. This condition is called aneuploidy which is caused by non disjunction of the chromosomes during meiosis (or mitosis). Fifty percent of first trimester spontaneous abortions are due to chromosome abnormalities. Animals do not tolerate deviation from the normal number of chromosomes. An extra chromosome is called trisomy and a missing one is called monosomy. There are no known autosomal monosomies.
In humans, the most common surviving chromosome abnormality is Down Syndrome (a.k.a. trisomy 21) which is due to an extra chromosome #21, the smallest chromosome (yes, it is smaller than #22). This causes the least imbalance but these children are not normal. They have a reduced IQ, are developmentally delayed, usually have heart defects and gastrointestinal defects, have a higher incidence of leukemia, are hypotonic (floppy babies), have a higher incidence of Alzheimer disease, and have an increased number of respiratory infections. Trisomy 13 and 18 are also known to survive to be born occasionally but usually die within a few months of birth.
DOWN SYNDROME (TRISOMY 21) CHILD

KARYOTYPE OF TRISOMY 21 FEMALE
The rate of non disjunction is correlated with maternal age. The probability of a woman having a fetus with a chromosome defect increases with age. At the age of 35 years, the risk of miscarriage due to a procedure called amniocentesis becomes less than the risk of having a child with a serious chromosome abnormality. The test is done usually between 15 and 20 weeks of gestation. So it is at the age of 34 or 35 that most women are offered this test which is virtually 100% accurate. A needle is inserted into the amniotic sac, and fluid is withdrawn which contains fetal cells. These cells are then karyotyped to detect aneuploidy. The fluid is also analyzed to detect NTDs or other abnormal openings in the fetus. While the test sounds scary or bizarre, it is done on a routine basis by obstetricians specializing in maternal fetal medicine and it is a safe test if done by an experienced practitioner. The State of California approves Prenatal Diagnostic Centers such as the one at King Drew Medical Center.

Because younger women have more children, they have the most Down Syndrome babies (and other aneuploidies). Therefore, several years ago, the State of California implemented a simple blood screening called XMSAFP, (Expanded Maternal Serum Alphafetoprotein) done between 15 and 20 weeks gestation to detect aneuploidies and NTDs. Three different analytes in the mother's blood are measured and along with the age of the mother, a risk is determined by comparison with an extremely large sample of blood taken from women with normal and abnormal pregnancies. The data was collected by the Genetics Disease Branch over many years. This screening is only 66% accurate for Down Syndrome but is 99.9% accurate for NTDs. Ultrasound is another good prenatal test. It can tell accurately the gestational age, the number of fetuses, the location of the placenta and can detect many structural abnormalities. An ultrasound is always done prior to an amniocentesis and most clinics will schedule at least one during each pregnancy.
Sex Chromosome Abnormalities
Aneuploidy involving the X and Y chromosomes is more common in humans since the results are less devastating than autosomal aneuploidies. This is because the Y carries very few genes and, if you have more than one X, the rest are inactivated and only one is functioning in each cell. So women have only one functional X even though they have two X chromosomes. They are one kind of "genetic mosaic." At about the 100 cell stage or less, either the paternal X or the maternal X is turned off. Since it is random which one, the human female has some cells in which the paternal X is functional and the maternal X is not or vice versa.
The only known monosomy is monosomy X, it is also known as Turner Syndrome. Turner females are very short, and due to edema when a fetus, they have webbing of the neck and high arched finger and toe nails, they have non functioning ovaries and are therefore sterile, they may have horseshoe shaped kidneys and often have heart problems. Their behavior is somewhat unique and they tend to have spatial perception problems. The lost X is generally that of the father and so is not correlated with maternal age.
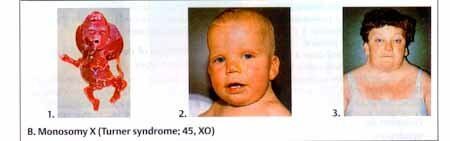
TURNER SYNDROME (45,X)
Klinefelter males are XXY. They are males because the testes determining gene (TDF/SRY) is on the Y chromosome. One of their two X's is inactivated just as in the human female with her two X chromosomes. Klinefelter males are tall, sterile, have hypogonadism, have gynecomastia, broad hips, and may have a slightly lower IQ compared to their normal sibs. Klinefelter and triple X are conditions which are associated with advanced maternal age of the mother.
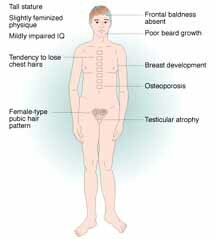

KLINEFELTER MALE AND 47,XXY KARYOTYPE
XXX, triple X females inactivate two of their X's. For the most part, they are normal and fertile but they are taller than their normal sisters, shy, and may be a little slow in school.
XYY males obviously arise from non disjunction in the sperm. They appear to be normal, are taller and may have a slightly reduced intelligence compared with their normal brothers.
Sex Determination
The Y chromosome carries the gene for testis determination (SRY gene). In developing embryos, the gonads and external genitalia are undifferentiated until about 7 - 8 weeks gestation. If the SRY gene is present, the gonads will go on to form testes, if not an ovary will form. The female is the default sex. There are several levels of sexual differentiation: chromosomal sex (XX or XY), gonadal sex (testes or ovary), internal plumbing sex (fallopian tubes, uterus or vas deferens, seminiferous tubules, epididymis), external plumbing sex (labia, clitoris or penis, scrotum) and psychosocial sex (which sex we feel we are). Most of the time we call a person male or female (the phenotype) by the external plumbing but that may not be consistent with the chromosomes or the gonads.
There are 46,XY individuals who have testes make male hormones but fail to make androgen receptors (this gene is on the X chromosome). Due to the lack of androgen receptors the individual never forms male internal or external genitalia. This condition is inherited as an XR and is called Androgen Insensitivity Syndrome (AIS). Testes make androgens (male hormones) and also a hormone called the anti-Mullerian hormone (AMH) which prevents the development of female internal reproductive organs (internal plumbing). This is why those 46,XY individuals with Androgen Insensitivity do not develop internal male plumbing nor internal female plumbing. They appear externally to be normal females with breast development but they have a blind vagina and are taller than their 46,XX sisters because of the height genes on their Y chromosome. They are normal but fail to menstruate at puberty and so come to the doctor's office. They also have scant axillary and pubic hair. When the condition is discovered, their gonads (testes) are removed to prevent them from developing gonadal blastoma (cancer).Testes are meant to be outside the body and when in the body cavity they tend to become cancerous. They usually lead their life as a normal female except for being infertile.
There are several genetic disorders which result in ambiguous genitalia or in genitalia of one sex but gonads of the other. Congenital Adrenal Hyperplasia (CAH) is an adrenal enzyme deficiency inherited as an AR disorder. It results in female embryos becoming masculinized due to excess androgens produced by the adrenal gland. The external genitalia of these females resembles male external genitalia. However, they are 46,XX and have female internal reproductive organs. Depending on the circumstances some are brought up as females and some as males. There is considerable debate on whether they should be given a chance to decide for themselves when they are older which sex they prefer to be. Since their brains have been exposed to androgens there is considerable evidence that their behavior is more male-like. Another disorder which results in ambiguous genitalia is called 5-alpha-reductase deficiency and is an AR disorder. This results in 46,XY fetuses having ambiguous genitalia due to the lack of dihydrotestosterone (DHT). DHT is the male hormone responsible for the external genitalia of males. It is made from testosterone by 5-alpha-reductase. When the enzyme is absent, the fetus cannot make normal male external genitalia.
We also are beginning to gather evidence that homosexuality may in most cases be a genetically controlled trait. (You will have to take my course in human genetics to learn more).

